It wasn’t a red carpet moment, but it made headlines just the same.
In a candid interview, pop icon Miley Cyrus revealed she had experienced an “excruciating” ovarian cyst rupture—an intensely painful, often underreported gynecological event that affects millions of women but rarely commands serious attention. Her admission, both vulnerable and unfiltered, struck a nerve: not just because of who she is, but because of how rarely public figures speak frankly about reproductive pain.
Ovarian cysts are remarkably common, and yet the suffering they cause often slips through the cracks of both pop culture and clinical practice. Cyrus’s revelation cast a spotlight on a medical issue that continues to be minimized, misdiagnosed, and misunderstood—an issue that says as much about healthcare as it does about celebrity.
What Is an Ovarian Cyst—and Why It Matters
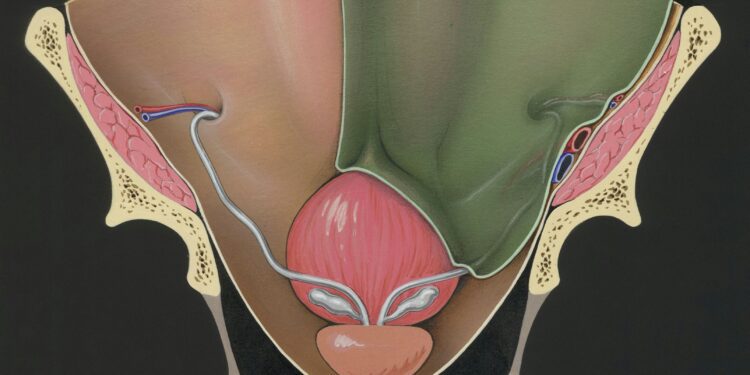
An ovarian cyst is a fluid-filled sac that develops on or inside an ovary. Most are benign and asymptomatic, but others can rupture, twist (a condition known as ovarian torsion), or cause significant bleeding and pain.
According to the Cleveland Clinic, ovarian cysts affect a majority of women at some point during their reproductive years. Yet because symptoms—pelvic pain, bloating, irregular periods—overlap with many other conditions, cysts are frequently dismissed or misdiagnosed.
That misdiagnosis can be costly. A ruptured cyst can mimic appendicitis or ectopic pregnancy and, in rare cases, may lead to hemorrhage and emergency surgery. Despite these risks, women reporting such pain are often met with skepticism or told they’re overreacting.
Miley Cyrus’s choice to name the pain—publicly—stands in sharp contrast to the medical system’s long-standing habit of silencing it.
The Diagnostic Dismissal of Women’s Pain
The phenomenon isn’t new. Studies have consistently shown that women’s pain is often taken less seriously than men’s. A landmark study in Academic Emergency Medicine found that women presenting with abdominal pain waited 33% longer than men to receive analgesics in the ER.
When it comes to reproductive pain—such as that from endometriosis, fibroids, or ovarian cysts—the problem is even more acute. These conditions often require imaging, specialist referrals, or laparoscopy to confirm—but are frequently reduced to “menstrual cramps” or anxiety in routine clinical encounters.
In pop culture, that erasure is compounded. Gynecological suffering is either played for laughs or completely ignored. Until a star like Cyrus says otherwise.
The Power of Celebrity Disclosure
Celebrities have long influenced health narratives—Angelina Jolie’s BRCA gene testing, Selena Gomez’s lupus diagnosis, even Michael J. Fox’s Parkinson’s advocacy. When a figure like Miley Cyrus discusses ovarian pain, it elevates the issue into mainstream conversation.
According to Healthline, online searches for “ovarian cyst symptoms” spiked after Cyrus’s interview. That spike, while fleeting, reflects something powerful: public validation for silent suffering.
But it also raises questions. Why does it take celebrity pain to draw attention to ordinary experiences? Why must a famous body become the proving ground for medical legitimacy?
The answer is complex—but ultimately rooted in how deeply society underestimates female health concerns.
A Public Health Issue Hiding in Plain Sight
Ovarian cysts are part of a broader pattern of reproductive neglect. Endometriosis affects 1 in 10 women of reproductive age and takes an average of 8 years to diagnose. Polycystic ovary syndrome (PCOS) affects 1 in 5 and is linked to infertility, metabolic disorders, and mental health issues—yet remains vastly underdiagnosed.
These are not fringe conditions. They are population-level health burdens. And they are routinely overlooked.
Part of the problem lies in education. Many women are not taught to recognize what abnormal pain looks like, and many providers are not trained to look beyond basic symptoms. A 2020 study in BMJ Open found that only 35% of general practitioners felt confident managing gynecological pain without a specialist.
The system, in other words, is not just under-informed. It is underprepared.
The Need for a Cultural and Clinical Shift
To move forward, we need more than awareness. We need accountability.
That means increasing investment in women’s health research, which currently receives less than half the funding of male-dominated disease areas. It means revising medical school curricula to prioritize pain equity and reproductive diagnostics. And it means listening—really listening—to patients when they describe their pain.
Public figures can help normalize the conversation. But structural change must follow.
Conclusion: From Pain to Power
Miley Cyrus didn’t ask to become a spokesperson for ovarian cysts. But her choice to speak out disrupted a silence that has gone on too long.
Her story is not unique. It is, in fact, painfully common. But in the echo of her words, there’s a call—to patients, to providers, to policymakers—to stop treating gynecological pain as a footnote.
Because for too many women, the pain is real, the diagnosis is delayed, and the silence is deadly.
It’s time to listen.
And more importantly, it’s time to act.