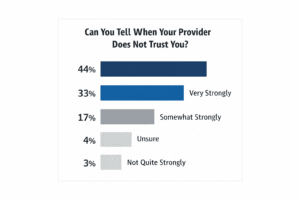
Question asked:
“How strongly do you believe that you can tell when your provider does not trust you?”
Key findings (n = 246):
-
77% of respondents report they can tell strongly or very strongly when a provider does not trust them.
-
Only 7% report little to no ability to detect distrust.
-
17% remain unsure, suggesting ambiguity rather than neutrality.
Interpretation:
Perceived trust is not subtle for most patients. A large majority believe they can reliably sense when a clinician doubts their honesty, adherence, or intentions. This suggests that provider trust—or lack thereof—is experienced as an emotionally salient signal, not a background variable.
A. Implications for Patients
-
Reduced Disclosure
-
Patients who sense distrust may withhold symptoms, medication nonadherence, or social factors.
-
This increases diagnostic error and undermines shared decision-making.
-
-
Emotional Withdrawal
-
Perceived distrust activates shame and defensiveness, especially in chronic pain, mental health, obesity, and substance-use contexts.
-
Patients may disengage silently rather than confront the issue.
-
-
Care Avoidance
-
Repeated experiences of distrust can lead patients to delay care, switch providers, or rely on non-clinical sources (online forums, influencers).
-
B. Implications for Physicians
-
Unintentional Signaling
-
Micro-behaviors (tone, interruptions, chart-focused attention, skepticism framing) may communicate distrust even when none is intended.
-
These signals often operate below conscious awareness.
-
-
Clinical Efficiency Paradox
-
Distrust may feel time-saving (“cutting through the story”), but it often costs time later through repeated visits, nonadherence, and conflict.
-
-
Burnout Feedback Loop
-
Distrust erodes relational satisfaction for clinicians, increasing emotional exhaustion and reinforcing cynical practice patterns.
-
C. System-Level Insight
-
Trust should be treated as a measurable clinical variable, not a “soft skill.”
-
Surveys like this can inform:
-
clinician training
-
patient-experience metrics
-
value-based care incentives
-
AI-assisted documentation and communication tools
-