The most consequential Alzheimer’s intervention may arrive decades before the diagnosis — and long before the billing code.
Brain health and dementia risk reduction have moved back into the center of clinical and policy conversation over the past two weeks, driven by renewed discussion of multi‑domain cognitive interventions, blood‑based biomarkers, and longitudinal prevention models circulating across research journals, specialty meetings, and health investment briefings. The intellectual center of gravity is shifting away from late‑stage treatment and toward upstream risk modification. Guidance and evidence reviews compiled by organizations such as the National Institute on Aging at https://www.nia.nih.gov and consensus summaries from expert commissions published in journals like The Lancet at https://www.thelancet.com increasingly frame dementia as partially modifiable rather than purely inevitable. For physician‑executives and healthcare investors, the tension is operational. Prevention science is accelerating. Delivery and payment architecture are not
The prevention thesis rests on convergence rather than breakthrough. Vascular risk control, metabolic health, hearing correction, sleep quality, cognitive engagement, and physical activity all show directional association with reduced dementia incidence in longitudinal cohorts. Multi‑domain intervention trials — including large lifestyle and risk‑factor modification studies indexed through https://pubmed.ncbi.nlm.nih.gov — suggest that structured combinations of these measures can slow cognitive decline signals in at‑risk populations. The effect sizes are real and modest. Modest effects matter at population scale and frustrate drug‑style expectations.
Evidence hierarchy complicates translation. Randomized prevention trials in cognition are long, expensive, and methodologically fragile. Adherence drifts. Contamination occurs. Control groups change behavior. Outcome measures are noisy. Surrogate endpoints — imaging changes, biomarker shifts, cognitive composites — stand in for hard dementia outcomes because hard outcomes take too long. Payers and regulators remain cautious when surrogates lead.
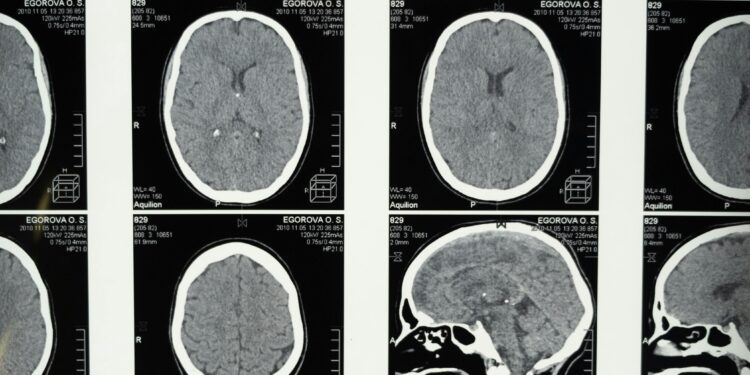
Biomarker development is compressing the timeline between pathology and detection. Blood‑based amyloid and tau assays, neurofilament light chain measurements, and inflammatory markers are increasingly studied as early risk indicators, with validation papers appearing in major journals and summarized in research updates from agencies such as the National Institutes of Health at https://www.nih.gov. Earlier detection improves prognostic precision and raises ethical and financial questions simultaneously. Risk knowledge without definitive intervention creates clinical ambiguity.
Second‑order clinical effects are already visible in specialty practice. Memory clinics are seeing more asymptomatic or mildly symptomatic individuals seeking risk profiling rather than diagnosis. Neurology workflows shift toward longitudinal counseling and risk discussion. Primary care absorbs more cognitive screening and referral coordination. Time demand rises before treatment options fully mature.
Payment design lags prevention logic. Fee‑for‑service systems reimburse diagnosis and procedure more reliably than longitudinal risk modification. Cognitive counseling, lifestyle coaching, and risk‑factor optimization programs often sit outside robust reimbursement pathways cataloged by the Centers for Medicare & Medicaid Services at https://www.cms.gov. Value‑based contracts theoretically reward prevention but require multi‑year attribution stability that many contracts do not sustain.
Investors see opportunity in the gap. Brain health platforms, digital cognitive training programs, remote monitoring tools, and biomarker testing firms position themselves as infrastructure for early detection and intervention. Evidence for many digital cognitive interventions remains mixed, with systematic reviews and meta‑analyses published in journals indexed through PubMed frequently showing heterogeneous effects. Engagement durability, not initial efficacy, is the limiting variable.
There is a counterintuitive behavioral dimension. Risk disclosure does not uniformly motivate protective behavior. Some patients increase exercise, dietary discipline, and cognitive engagement when confronted with quantified dementia risk. Others disengage under perceived inevitability. Behavioral response curves are not linear functions of risk information. Preventive neurology is also preventive psychology.
Workforce implications are subtle and undercounted. Effective dementia risk reduction depends on sustained counseling, coaching, and monitoring — activities distributed across physicians, advanced practice clinicians, psychologists, and allied health professionals. Workforce models built for episodic specialty care struggle with continuous preventive engagement. Capacity becomes the constraint before science does.
Hearing loss illustrates the complexity of modifiable risk translation. Epidemiologic studies consistently associate untreated hearing impairment with higher dementia risk. Hearing correction reduces isolation and cognitive load. Yet hearing aid adoption remains uneven, despite regulatory changes expanding over‑the‑counter device availability described by the FDA at https://www.fda.gov/medical-devices/hearing-aids. Technology access does not guarantee behavioral adoption.
Sleep science offers a parallel example. Associations between sleep fragmentation, sleep apnea, and neurodegenerative risk appear repeatedly in cohort studies and mechanistic research. Sleep intervention improves quality of life and cardiometabolic outcomes. Direct dementia risk reduction remains probabilistic rather than proven. Clinicians must speak in probabilities while patients prefer certainties.
Public messaging often compresses complexity into slogans — “prevent Alzheimer’s,” “protect your brain” — while the underlying evidence supports risk reduction, not elimination. The distinction matters. Overstatement erodes credibility when outcomes vary. Understatement reduces engagement. Communication strategy becomes a clinical tool.
Policy frameworks are experimenting cautiously. National dementia strategies published by multiple countries and summarized in global health policy repositories increasingly include prevention pillars alongside care infrastructure. Implementation funding tends to favor diagnostics and care delivery more than lifestyle intervention scaling. Prevention is endorsed rhetorically and funded selectively.
For health systems, the economic paradox is persistent. Successful dementia prevention reduces long‑term cost and near‑term revenue tied to advanced disease management. Institutions dependent on downstream service revenue experience prevention as financial ambiguity. Population health models mitigate but do not erase this tension.
Scientific uncertainty remains irreducible. Dementia is heterogeneous. Alzheimer’s pathology overlaps with vascular, inflammatory, and mixed etiologies. Risk models explain variance, not destiny. Precision prevention remains aspirational.
What is changing is not certainty but posture. Dementia is increasingly treated as a risk trajectory that can be bent, not a cliff that cannot be avoided. Bending trajectories requires time horizons longer than most payment cycles and investment models comfortably allow.
Prevention advances in gradients. Systems prefer thresholds. The friction between those two logics is where brain health policy now lives.