Every time a fluoroquinolone molecule glides across a pharmacy counter, it carries two possibilities: cure or instruction manual for the enemy.
For most of the 1990s, ciprofloxacin—“Cipro” in ER shorthand—embodied antibiotic swagger: broad-spectrum, orally bioavailable, fast. But beginning in the early 2000s, microbiologists noticed a disquieting trend: hospitals that used more Cipro recorded faster rises in multidrug-resistant infections. Correlation invited skepticism—until basic-science teams, armed with genomic sequencers and mouse models, revealed a startling mechanism. At sub-lethal doses, fluoroquinolones activate the bacterial SOS response, a DNA-repair circuit that paradoxically floods genomes with mutations, some of which encode drug resistance.
1 | From Petri Dish Clues to Mechanistic Proof
The first hints surfaced in 2010, when Molecular Cell researchers showed that Escherichia coli grown in one-tenth the inhibitory concentration of Cipro accumulated multidrug resistance via reactive-oxygen mutagenesis (Molecular Cell). Critics said lab broth isn’t a bloodstream. So the same group migrated to a mouse thigh-infection model, proving that Cipro-treated bacteria needed a functional SOS regulator (RecA) to evolve resistance in vivo (PNAS Hub Study). When RecA was genetically silenced, mutation rates plunged six-fold, and no resistant colonies emerged.
By 2019, a Nature Communications paper generalized the finding: fluoroquinolones damaged DNA in persister cells, and the ensuing SOS surge accelerated resistance even to unrelated drugs (Nature Communications). The study coined the term “collateral mutagenesis” to describe how one antibiotic sows the seeds for defeating others.
2 | Clinical Footprints—Heteroresistance Comes into Focus
Bench results are unsettling; bedside evidence is damning. A 2024 surveillance of 100 Acinetobacter baumannii isolates found 86 % were ciprofloxacin-resistant, most harboring plasmid-mediated quinolone-resistance genes (JAC-AMR). Parallel work at Zhejiang University Hospital linked Cipro exposure to mepA overexpression and membrane-potential collapse, producing a stealthy form of partial resistance called heteroresistance—susceptible by standard tests yet harboring resistant subclones (AAC Insight).
Why does heteroresistance matter? Because clinicians may unknowingly prescribe the very drug nurturing the resistant minority, allowing it to dominate mid-therapy and trigger treatment failure.
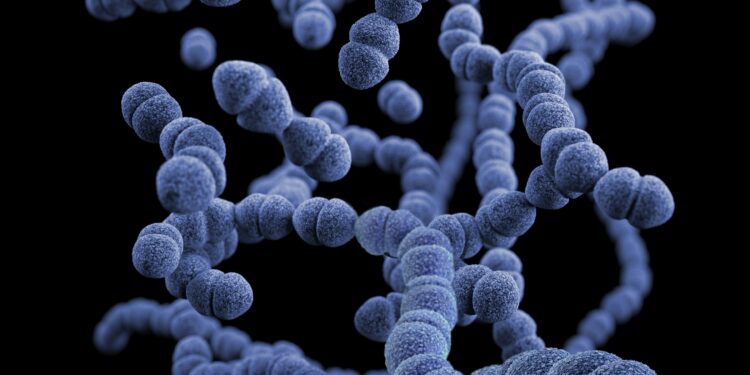
3 | How the SOS Response Turns Medicine on Its Head
3.1 DNA Damage → RecA Activation
Fluoroquinolones block DNA gyrase, creating double-strand breaks. Bacteria sense the crisis and auto-cleave the LexA repressor, unleashing the SOS regulon of more than 40 genes—including error-prone polymerases.
3.2 Mutagenic Repair
Polymerase V (UmuDC) races to patch breaks but lacks proofreading. Every hurried insertion risks a misspelling, some of which fortify efflux pumps or tweak drug targets.
3.3 Population Roulette
Within a single overnight culture, millions of genomic lottery tickets are printed. The one that nullifies Cipro’s attack turns a subpopulation into tomorrow’s dominant strain.
King’s College mathematicians modeled this cascade and estimated a 70 % shorter timeline to high-level resistance when bacteria experience fluctuating low-dose exposure versus a single lethal hit.
4 | Reconstructing the Research Journey
- Epidemiology Flags a Paradox
Pharmacy-wide data in U.K. hospitals revealed a dose-response curve: each additional DDD (defined daily dose) of fluoroquinolone correlated with a 3 % annual rise in MRSA. - In Vitro SOS Screens
Fluorescent reporter plasmids inserted into E. coli glowed green under Cipro, quantifying SOS activity versus drug concentration. - In Vivo Validation
Mouse models introduced isogenic strains differing only in recA; only the SOS-competent bacteria evolved resistance under therapy. - Whole-Genome Sequencing
Oxford Nanopore platforms mapped mutation spectra, confirming a spike in G:C→T:A transversions, signatures of ROS damage. - Clinical Isolate Genomics
Hospitals forwarded failure-case isolates; sequencing revealed identical SOS-linked mutational footprints, closing the loop from bedside back to bench.
5 | Patient Vignettes—Resistance in Real Time
5.1 ICU Spiral
A 67-year-old COPD patient admitted with urinary sepsis received intravenous Cipro after cultures grew E. coli marked “susceptible.” Fever broke, then roared back on day four. A repeat culture revealed Cipro MIC had jumped eight-fold. Genomic analysis later showed a gyrA Ser83Leu mutation plus up-regulated SOS genes—classic quinolone-driven escape.
5.2 Traveler’s Regret
A backpacker in Thailand picked up traveler’s diarrhea, popped over-the-counter Cipro tablets at half-dose “to be safe,” and seeded her gut with fluoroquinolone-heteroresistant Salmonella. Back home, the bug dodged azithromycin and ceftriaxone, forcing a four-week carbapenem course.
6 | Stewardship Shake-Ups—What Now?
- Kill It Fast or Not at All
Infectious-disease societies now argue for high-intensity, short-duration dosing to outrun SOS induction, akin to how oncologists pulse chemotherapy. - RecA Blockade as Adjuvant
Biotech start-up EvolvereBio is trialing a RecA inhibitor that, when paired with Cipro, cuts emergent resistance by 95 % in murine pyelonephritis models. - Diagnostics for Heteroresistance
UC San Diego engineers built a microfluidic chip that detects resistant subpopulations in under two hours, outperforming standard MIC tests unable to spot heteroresistance (BMC Microbiology). - Policy Nudges
Sweden slashed outpatient fluoroquinolone scripts 43 % in five years by making prescribers justify choices in EHR pop-ups—a model now piloting across the EU.
7 | Rethinking Drug Design—Fluoroquinolones 2.0?
Medicinal chemists are engineering “silent quinolones” that kill bacteria without SOS activation. Early candidates replace the C-8 fluorine, dampening ROS generation while maintaining topoisomerase binding. A 2023 Cell Chemical Biology preprint showed these analogs eradicate E. coli at nanomolar doses without triggering recA fluorescence. Human trials begin in 2026.
8 | The Unanswered Questions
- Cross-Kingdom Spillover: Does sub-lethal Cipro in agricultural runoff accelerate resistance in environmental microbiomes that later donate plasmids to pathogens?
- Viral Co-infections: Early data hint that SOS activation increases prophage induction, potentially transferring resistance genes across species.
- Therapeutic Windows: How narrow is the dose that kills pathogens but dodges SOS? Pharmacodynamic curves urgently need updating.
Conclusion | Turning the Lens Back on a Trusted Pill
Ciprofloxacin will remain in the pharmacopoeia—it saves too many lives to vanish. But like fire, its utility depends on containment. The science now tells a consistent story: half-measures with fluoroquinolones convert microbes into gamblers, and the house—modern medicine—risks losing. Stewardship, surveillance, and smarter molecules form the new three-pillared defense.
The next time a mild infection tempts a quick Cipro script, physicians and patients alike might recall the boomerang hidden in every blister pack: an SOS siren summoning tomorrow’s superbug. In the microbial casino, fluoroquinolones taught us the rules late; now we must play—and prescribe—accordingly.