In a bustling hospital in Addis Ababa, Ethiopia, patients queue anxiously, nurses rush between packed wards, and health officials tally numbers with grim precision. It’s early May 2025, and another public health nightmare is quietly but persistently unfolding: Mpox—formerly known as monkeypox—is surging back across Africa, hitting at least 19 nations with alarming speed. Over 52,000 confirmed cases have been reported this year alone, thrusting the continent back into the grim spotlight of global health emergencies. Meanwhile, desperate pleas from the Africa Centers for Disease Control and Prevention (Africa CDC) for vaccines echo unanswered. In a world weary of pandemics and fatigued by geopolitical discord, Africa finds itself not merely battling a virus but also confronting the stark reality of geopolitical abandonment.
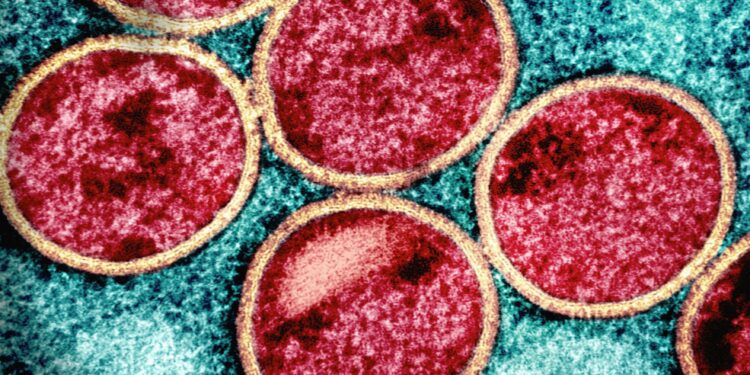
Mpox isn’t new. Since its initial discovery in the 1970s, scattered outbreaks have periodically emerged across central and western Africa. However, recent developments are deeply concerning. The sheer scale and rapid spread of the current outbreak—in nations such as Ethiopia, Malawi, Nigeria, and South Africa—underscore a dangerous new chapter. African public health officials are urgently calling for increased vaccine supplies, pointing to an unsettling disparity: While wealthy nations have stockpiled treatments, African countries face crippling shortages.
The Africa CDC’s recent statements highlight this imbalance vividly. Dr. Ahmed Ogwell, the interim director, stressed in an urgent press briefing that “our ability to control this outbreak relies heavily on equitable access to vaccines. We need immediate global support.” The response from international allies, however, has been muted and inconsistent, overshadowed by more immediate geopolitical crises and political concerns.
Adding a layer of complexity, former U.S. President Donald Trump’s enduring legacy on immigration policies continues to affect perceptions among African nations regarding American reliability as a public health partner. Trump’s stringent anti-immigration stance, epitomized by policies aimed explicitly at restricting entry from numerous African countries, left an enduring bitter taste among many African governments and citizens. Such policies, though largely symbolic at their inception, have had lasting practical implications, including increased hesitance among African leaders to openly rely on or trust American-led initiatives, even in matters as universally critical as public health.
This skepticism toward U.S. intentions is compounded by ongoing vaccine distribution inequities. African nations watched in frustration as developed countries rapidly secured large supplies of Mpox vaccines, while their own urgent appeals went unmet. The unequal global vaccine distribution mirrors previous disparities seen during the COVID-19 pandemic, reinforcing narratives of neglect and abandonment. Viral social media content, especially on platforms like TikTok, has amplified voices of frustration and calls for greater equity, highlighting both the severity of the outbreak and perceived injustices in global vaccine distribution.
Mpox’s resurgence in Africa also exposes chronic vulnerabilities within local health infrastructures, exacerbated by limited international support. In Malawi, for example, frontline healthcare workers—already overwhelmed by the ongoing battle against HIV/AIDS and tuberculosis—are stretched perilously thin. Vaccine scarcity only intensifies these systemic stresses, amplifying the crisis. Public health experts argue this cycle—underfunded systems, reactive rather than proactive global responses, and persistent vaccine inequities—creates fertile ground for recurring outbreaks.
Furthermore, the reluctance of some African communities to trust vaccines, stemming from historical mistrust and contemporary geopolitical tensions, complicates response efforts. The misinformation epidemic, accelerated by rapid digital dissemination, fuels vaccine hesitancy even as supplies slowly begin trickling in. Healthcare providers across affected regions report increased resistance among populations already skeptical of external interventions due to historical exploitation or neglect.
The Trump-era immigration policies have significantly influenced these attitudes, reinforcing skepticism toward Western interventions. Social media across Africa is replete with sentiments questioning why countries should rely on aid from nations perceived as hostile or indifferent. For many Africans, the echoes of Trump’s divisive rhetoric reverberate loudly in moments of crisis, reinforcing suspicion and doubt toward even well-intentioned health interventions.
Observers argue that the United States’ global health diplomacy requires urgent recalibration. Effective responses to health crises must transcend domestic political agendas and short-sighted immigration debates. A failure to recognize and address these intertwined dynamics risks undermining decades of public health advancements and further alienating critical international partners.
Dr. Olufemi Ayodele, a health policy researcher based in Lagos, Nigeria, explained, “Public health crises are not isolated medical events. They are shaped significantly by political realities. Africa’s current experience with Mpox starkly illustrates the consequences when geopolitical tensions overshadow collective humanitarian goals.”
As Africa battles Mpox anew, the world faces a pivotal moment. Lessons from the COVID-19 pandemic remain distressingly unlearned. Global solidarity, equitable vaccine distribution, and depoliticized health initiatives are still distant ideals rather than operational realities. Continued neglect and geopolitical maneuvering threaten not only the health of African populations but global stability itself, as unchecked outbreaks inevitably become global threats.
The international community, particularly Western nations, must reevaluate their approach to global health, prioritizing long-term relationships built on trust, equity, and mutual respect rather than short-term political expediencies. The resurgence of Mpox provides a sobering reminder: viruses do not recognize political borders or immigration policies. Health crises demand comprehensive global cooperation, unfettered by political divides.
In conclusion, Africa’s Mpox resurgence symbolizes more than a health emergency; it highlights profound global inequities and simmering geopolitical tensions exacerbated by exclusionary policies. As the continent grapples with vaccine shortages and wavering international support, the world must decide whether to prioritize humanitarian responsibility over political isolationism. The choice, stark and urgent, will dictate not only Africa’s health future but the broader narrative of global health security in an interconnected yet politically fragmented world.