Infection risk has returned to everyday consciousness, not as a pandemic emergency but as a background condition of modern life.
Search and social-media discourse over the past two weeks show sustained engagement around immune system support, cold and flu prevention, norovirus outbreaks, respiratory virus season forecasts, and “how to boost immunity” queries, with recurring reference traffic to federal guidance from the Centers for Disease Control and Prevention at https://www.cdc.gov and global surveillance updates from the World Health Organization at https://www.who.int. The pattern is steady rather than sensational. It reflects a behavioral afterimage of recent pandemic years combined with seasonal pathogen circulation and a permanently heightened awareness of transmission dynamics. Immune health has migrated from textbook concept to consumer-facing category, and that migration carries consequences for care delivery and policy design.
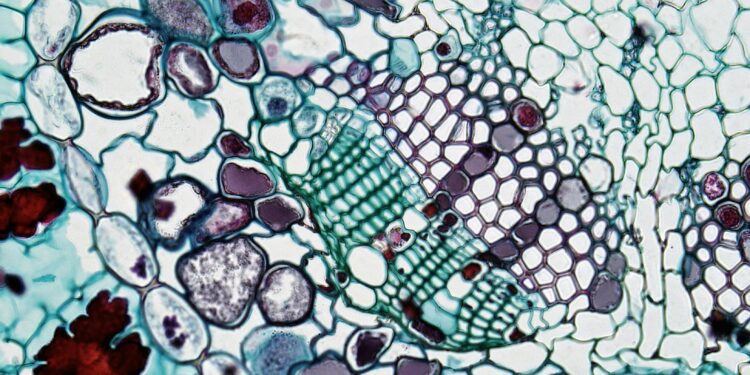
The popular vocabulary of immunity is expansive and imprecise. The clinical reality is narrower and more conditional. Host defense is shaped by vaccination status, prior exposure, age, comorbidity, nutrition, sleep, and chance. Yet the commercial immune-health market — supplements, functional foods, testing panels — behaves as if immune performance were continuously tunable through retail intervention. Regulatory boundaries described by the Food and Drug Administration at https://www.fda.gov distinguish between disease claims and structure-function claims, but consumer interpretation often collapses the distinction. Suggestion becomes promise in transit.
Prevention behavior has become more elastic since the pandemic, but not uniformly more durable. Masking, testing, and isolation norms now oscillate with perceived threat rather than official declaration. Syndromic surveillance dashboards published by public-health agencies — including respiratory virus tracking tools at https://www.cdc.gov/respiratory-viruses — influence behavior among the attentive and bypass the disengaged. Risk response has stratified by information diet. That stratification complicates forecasting models that assume homogeneous behavioral adjustment.
Vaccination remains the most reliable large-scale immune intervention and the most behaviorally contested. Seasonal influenza, updated COVID formulations, and adult booster recommendations generate recurring waves of attention tied to advisory committee updates and coverage guidance posted at https://www.cdc.gov/vaccines. Uptake variability now reflects not only access but fatigue. Recommendation density has increased; marginal persuasive power has not. Each additional recommended dose competes with accumulated skepticism and logistical friction.
There is a counterintuitive utilization effect in heightened infection awareness. As mild symptom vigilance rises, diagnostic testing demand increases, which raises short-term utilization even when severe disease rates remain stable. Urgent care and retail clinic volumes often reflect perception curves as much as pathogen curves. Claims analyses published through federal datasets at https://www.hcup-us.ahrq.gov show how respiratory-season utilization patterns widen at the low-acuity end before they shift at the high-acuity end. Systems feel the surge before outcomes justify it.
Workplace infection policy has entered a hybrid phase. Employers maintain flexible sick-leave and remote-work norms in some sectors while reverting to pre-pandemic attendance expectations in others. Occupational health guidance from agencies such as the Occupational Safety and Health Administration at https://www.osha.gov provides baseline frameworks but leaves implementation detail to organizations. The result is policy heterogeneity within the same labor market. Transmission risk and income security are now partly employer-specific variables.
Healthcare facilities face a related trade-off between infection control rigor and operational throughput. Enhanced ventilation, screening protocols, and isolation capacity improve resilience and raise fixed cost. Infection-prevention standards described by professional bodies and summarized in federal guidance at https://www.cdc.gov/infectioncontrol are clearer than their financing pathways. Prevention infrastructure is funded as overhead until an outbreak reframes it as necessity. Budget lines tend to follow crises, not probabilities.
The immune-supplement economy deserves scrutiny beyond its marketing claims. Systematic reviews indexed through the National Institutes of Health at https://ods.od.nih.gov show mixed or modest evidence for many widely used supplements. Heterogeneity in product quality and dosing further complicates interpretation. Consumer demand persists because perceived agency has value independent of clinical effect size. The desire to act is itself a market force.
Second-order antimicrobial effects are easy to miss in prevention conversations. Heightened infection anxiety can increase inappropriate antibiotic demand for viral illness, despite stewardship campaigns. Stewardship frameworks promoted by the CDC at https://www.cdc.gov/antibiotic-use aim to counter this drift, but prescribing behavior remains sensitive to patient expectation and time pressure. Resistance patterns are shaped as much by outpatient habits as inpatient protocols.
Norovirus and other gastrointestinal outbreaks illustrate another systems tension: reporting visibility versus behavioral response. Outbreak notices and institutional dashboards improve transparency and can produce localized overreaction — school closures, supply hoarding — when risk is poorly contextualized. Public-health communication must calibrate urgency without inducing distortion. Calibration is difficult under attention-driven media cycles.
Immunocompromised populations experience these dynamics differently. For patients with transplant, oncology, or advanced autoimmune disease, infection prevention remains a daily operational discipline rather than seasonal advice. Clinical guidance from specialty societies and federal resources at https://www.cancer.gov and related institutes emphasizes layered protection strategies that rarely translate cleanly into public messaging. Population-level simplification obscures subgroup necessity.
Digital epidemiology has expanded the data environment without resolving interpretation challenges. Wastewater surveillance, mobility data, and search-query trend models — discussed in public-health analytics literature indexed at https://pubmed.ncbi.nlm.nih.gov — offer earlier signals of pathogen spread. Earlier signals create earlier debate about response thresholds. Acting too soon looks alarmist; acting too late looks negligent. Signal lead time increases decision ambiguity before it reduces uncertainty.
Investors and operators increasingly treat infection prevention as infrastructure rather than episodic expense. Air-quality technologies, rapid diagnostics, tele-triage platforms, and decentralized testing services attract capital on the thesis that endemic respiratory risk is the new baseline. Some of these bets will prove durable. Others depend on memory of crisis that may fade faster than depreciation schedules.
Global equity questions persist beneath domestic trendlines. Vaccine access, antiviral availability, and surveillance capacity remain uneven across income gradients, as documented in global health reports at https://www.who.int/data. Pathogens travel faster than procurement reform. Preparedness is only as strong as the least prepared node in a connected system.
Immune health is now discussed with the language of optimization, but most meaningful gains still come from unglamorous measures: vaccination, ventilation, hygiene, paid sick leave, and credible communication. The tension between marketable optimization and boring effectiveness is unlikely to disappear. Public attention prefers novelty. Immune systems prefer consistency.
Infection prevention has moved from specialist domain to shared civic responsibility without acquiring stable civic consensus. That gap — between responsibility and agreement — is where most of the policy friction now resides.