A subtle upheaval unfolds in psychological services as algorithmic therapists converse with patients at odd hours and headsets transport trauma survivors back to their most feared memories in controlled simulations. Meanwhile, the National Health Service has onboarded more than 6 700 mental health professionals since July, marking a decisive investment in human capacity to complement burgeoning digital interventions.
That recruitment surge forms a key pillar of the forthcoming NHS Long Term Plan, which mandates expansion of talking therapies, crisis resolution teams and digital self-help tools through the NHS App. The introduction of AI-powered chatbots within that platform aims to provide immediate cognitive behavioural therapy exercises and mood monitoring without the wait for an appointment.
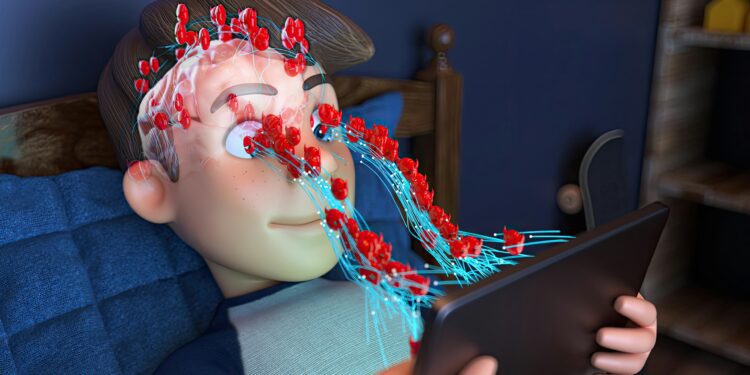
AI-Driven Therapy Applications
Conversational agents such as Woebot and Tess illustrate the promise of artificial intelligence in mental healthcare. In a randomized controlled trial, university students who interacted daily with Woebot for two weeks experienced a 20 percent greater reduction in depressive symptoms than peers receiving static informational material. Tess, deployed across several counselling services, delivered personalised coping strategies that yielded significant decreases in anxiety scores over a four-week period, according to a peer-reviewed study.
These AI platforms operate around the clock with minimal marginal cost per patient. They furnish psychoeducation, mood tracking and interactive journalling, thereby reducing stigma and lowering thresholds for initial help-seeking. Critics argue that predictive algorithms may oversimplify complex emotional narratives and fail to replicate the empathic attunement of human therapists. Moreover, data passing through third-party servers poses privacy risks if encryption standards prove inadequate or if patient consent does not explicitly cover secondary uses.
Virtual Reality Exposure Therapy
Virtual reality exposure therapy transports individuals into controlled simulations of traumatic or anxiety-provoking scenarios under therapist supervision. A meta-analysis of nine trials found that VRET produced a medium effect size (Hedges’ g = 0.62) in alleviating post-traumatic stress symptoms compared with waitlist controls. In a recent Veterans Affairs trial, pairing VR sessions with low-intensity transcranial direct current stimulation led to rapid symptom reductions after six sessions—outcomes comparable to twelve weeks of traditional imagery rehearsal therapy, as reported in JAMA Psychiatry.
Despite robust outcomes, practical barriers impede widespread adoption. High-resolution headsets and immersive software incur upfront costs exceeding several thousand pounds per unit. Clinicians require specialised training to administer exposure protocols safely. Reimbursement frameworks remain nascent, and in the absence of established billing codes insurers may not cover VR services. Furthermore, most trials focus on military or first-responder cohorts, leaving civilian applicability and cultural adaptation underexplored.
Workforce Expansion and Blended Care Models
The infusion of over 6 700 additional mental health professionals into NHS services reflects a strategic acknowledgement that technology complements rather than replaces human expertise. According to the Royal College of Psychiatrists, digital tools will serve as “front-door” options via the NHS App, but sustained improvements in patient outcomes depend upon integration with face-to-face therapies and multidisciplinary teams.
Training curricula for newly recruited psychologists, psychiatric nurses and allied professionals now incorporate modules on digital literacy, remote risk assessment and ethical frameworks governing algorithm-guided care. Academic institutions partner with tech developers to offer practicum placements in digital mental health labs, ensuring the next generation of practitioners grasps both humanistic counselling and data-driven intervention strategies.
Equity and Access Imperatives
Digital therapies promise to expand access, particularly for individuals in remote or underserved regions. However, without deliberate equity measures, such innovations risk deepening existing disparities. The World Health Organization cautions that digital health initiatives must address device affordability, broadband connectivity and digital literacy to achieve universal benefit. The NHS has commenced pilot programmes offering loaned devices, translation services and community workshops to foster engagement with AI therapy apps.
Globally, low- and middle-income countries regard AI and VR platforms as scalable solutions to long-standing shortages of mental health professionals. Yet most such applications originate in high-income settings, raising questions about cultural relevance and linguistic appropriateness. Collaborative development with local practitioners and participatory design methodologies can ensure that digital content resonates with diverse populations.
Emerging Research and Case Studies
Several pioneering programmes illuminate the evolving landscape. A consortium of European universities integrated Woebot into campus counselling services, reporting a 35 percent increase in help-seeker engagement and a marked decline in no-show rates for in-person appointments over six months, according to a published report. In Scandinavia, a clinic employing a VR public-speaking module for social anxiety disorder observed improved performance and reduced avoidance behaviour at six-month follow-up, as detailed in Behaviour Research and Therapy.
Cutting-edge research explores multimodal AI systems that synthesise text, vocal tone and facial expression data to tailor interventions dynamically. A recent arXiv preprint describes a socially assistive robot guiding participants through at-home mindfulness exercises, yielding anxiety reductions comparable to traditional workbook methods. Ongoing trials are examining federated learning approaches that train algorithms across decentralized patient data without compromising privacy.
Regulatory and Reimbursement Considerations
Regulators and payers must reconcile rapid technological innovation with safety, efficacy and equitable reimbursement. The National Institute for Health and Care Excellence has published draft guidelines for digital mental health interventions, outlining evidence thresholds for approval and recommending patient data governance standards. Meanwhile, the U.S. Centers for Medicare & Medicaid Services are exploring pilot reimbursement codes for VR exposure therapy and AI-guided cognitive exercises.
Policymakers face the challenge of balancing rigorous evaluation with timely access. Adaptive trial designs and real-world evidence collection may facilitate iterative approval processes. Data registries that track outcomes across digital and in-person modalities can inform ongoing policy refinement and ensure that funding aligns with demonstrable improvements in patient well-being.
Conclusion
The confluence of AI therapy applications, immersive virtual reality treatments and a bolstered clinical workforce heralds a new paradigm in mental healthcare delivery. Technology extends the reach and immediacy of services, yet the essence of therapeutic alliance and clinical judgment remains irreplaceable. As the NHS and global health systems adapt to blended care models, the ultimate measure of success will reside in equitable access, sustained patient outcomes and the preservation of empathy in every therapeutic encounter. Continuous innovation must proceed in tandem with robust governance to ensure that digital front doors lead to meaningful, compassionate and effective mental health support.