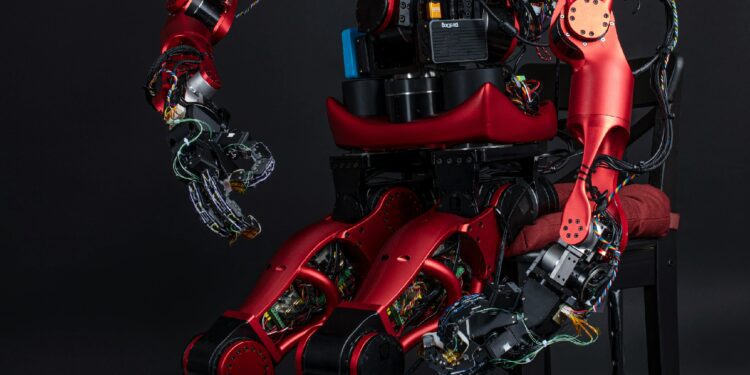
A whirr of mechanical arms and the soft glow of a console screen now guide surgeons’ hands toward incisions measured in millimetres rather than centimetres. Minimally invasive, robot-assisted surgery promises reduced trauma and faster recovery, yet its embrace of artificial intelligence and advanced hardware raises intricate questions about error rates, complication profiles and the shifting burden of responsibility.
In surgical practice, a complication denotes any unintended adverse event that prolongs recovery, inflicts additional harm or necessitates further intervention. Traditionally, metrics include infection, hemorrhage, organ injury and unplanned conversions to open procedures. Under robotic assistance, new classes of complications emerge: mechanical failures, software glitches and device-related injuries.
A retrospective study of nearly two thousand da Vinci procedures found a failure rate of approximately 0.38 percent—comprising device malfunctions and conversions to open surgery—though patient injury rates remained largely unchanged (failure rate). Another analysis uncovered seventy-eight adverse events in robotic laparoscopy over two years, including broken instrument tips and electrocautery failures (adverse events). By contrast, conventional laparoscopy in adnexal surgery showed a complication rate of 7 percent versus 6 percent for robotic cases—illustrating that automation does not universally reduce adverse outcomes (complication rate).
Mechanical and software failures now account for a significant share of robotic complications. Institution-wide audits report failure rates between 0.4 and 3.7 percent, including arm collisions, camera malfunctions and instrument fractures (failure rates). Electrosurgical injuries—once rare—now represent nearly 4 percent of reported incidents, over one-third requiring further intervention (electrosurgical injuries).
Human surgeons contend with skill variability, fatigue and cognitive overload, but they retain tactile feedback and intuitive judgment. Robots deliver tremor filtration and precise movements yet lack haptic sensation. Consequently, tissue tearing from excessive force may decline, while unrecognized thermal spread from electrocautery becomes more prevalent.
Cardiac surgery underscores these tensions. Early adopters criticised the da Vinci system’s performance on a constantly moving organ, noting a fourfold increase in complications during atrial-fibrillation ablations compared with manual techniques due to targeting challenges and a steep console learning curve (robotic surgery challenges). Conversely, in prostatectomy and gynecologic oncology, robots yield fewer complications—reduced blood loss, shorter hospital stays and lower thrombosis rates (shorter hospital stay).
As robotic platforms diffuse into community hospitals, training and oversight challenges escalate. Many residency programs offer only minutes of supervised console practice despite evidence that proficiency demands hundreds of cases (training challenges). Without rigorous credentialing, robotics’ rapid spread may paradoxically elevate complication rates in under-resourced settings.
Economic analyses reveal steep costs: each da Vinci system can exceed $2 million, with annual maintenance above $100 000 and disposable instruments adding thousands per case (device cost). Robotic procedures carry a $3 000–$6 000 premium over laparoscopy, translating into an 80 percent cost increase. Advocates cite reduced complication costs and shorter stays; critics warn marginal outcome gains seldom justify the capital outlay.
Accountability grows complex when devices malfunction. Current regulations classify surgical robots as Class II medical devices, subject to recalls and post-market surveillance (FDA recalls). Yet major device corrections sometimes proceed without timely surgeon notification, leaving operators unaware of known failure modes during operations (warning letter history).
To adapt, health systems must integrate robust error-reporting systems that combine machine logs, video review and structured incident analysis—shifting from blame to root-cause investigation (error-reporting systems). Next-generation robots promise haptic feedback, AI-guided visualization and partial autonomy for routine tasks. Each added autonomy layer demands rigorous verification, clinician–developer collaboration and enhanced training to manage novel failure points.
Robotic-assisted surgery stands at the crossroads of technological promise and practical challenge. Its precision and minimally invasive benefits coexist with distinct error modes, high costs and an evolving complication landscape. Ensuring patient safety and value requires addressing training deficits, refining design, strengthening reporting and critically evaluating cost-effectiveness. In tomorrow’s operating room, success depends not merely on mechanical arms but on the integrity of the systems that support, regulate and humanize them—thereby advancing surgical care without trading one set of risks for another.