The Body as Algorithmic Subject
The footage begins plainly. A montage of clothing struggles, physical discomfort, and slouched posture. The music is soft, deliberate. Then, a shift: hospital gowns, operating rooms, post-operative gauze. The final reveal—standing upright, arms relaxed, visibly relieved. Within days, the TikTok video surpassed 25 million views. Its subject, a young woman narrating her breast reduction experience, became a flashpoint for a digital public wrestling with the convergence of body image, gender expectations, and surgical intervention.
Media coverage from People Magazine quickly followed, chronicling how the video’s emotional arc resonated across a spectrum of users—young and old, male and female, those contemplating the same surgery and those confronting larger cultural narratives about bodily “normalcy” (source). What emerged was not merely a story about cosmetic surgery. It was a layered conversation about pain, visibility, credibility, and permission—who gets to alter their body, who gets to talk about it, and what it means when the internet responds.
Reclaiming the Clinical from the Cosmetic
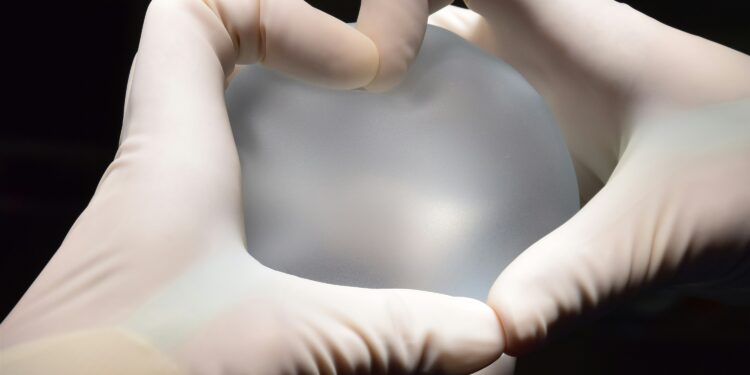
Breast reduction surgery occupies an unusual place in medical discourse. While often classified as a cosmetic procedure, it carries legitimate indications in physical medicine and rehabilitation. Patients commonly report chronic back pain, restricted mobility, bra strap grooving, intertrigo, and postural dysfunction—all of which respond to surgical correction. In most cases, such surgeries are not about vanity, but relief.
Yet insurance companies frequently deny coverage, arguing the procedure lacks “medical necessity.” This bureaucratic stance has forced countless women into protracted battles for reimbursement, simultaneously reinforcing the false assumption that breast reduction is discretionary.
By foregrounding these physical complaints—and narrating the emotional toll of living in a body that elicits both judgment and voyeurism—the viral video reshaped the public perception of the surgery. It did not glamorize transformation. It medicalized suffering, without apology. In doing so, it invited a broad reassessment of how we categorize medical need, particularly in relation to gendered anatomy.
The Aesthetic Gaze and the Risk of Overidentification
There is an inherent paradox in broadcasting personal medical decisions online. On one hand, such acts reclaim agency in spaces historically marked by silence or shame. On the other, they risk flattening experience into aesthetic satisfaction or voyeuristic curiosity.
Within hours of the video’s ascent, TikTok comments flooded with personal testimonies—some affirming, others voyeuristic. Many viewers thanked the poster for her “bravery,” but others interrogated her choices: Why not try physical therapy first? Were her breasts really that large? Couldn’t she have simply embraced her body?
The commentary reflects a cultural impulse to adjudicate bodies, especially female ones, according to communal standards rather than individual need. What should have remained a singular medical journey morphed, in digital space, into a referendum on femininity, medical legitimacy, and self-presentation.
Social Media as an Engine of Disclosure—and Distortion
Social media is a uniquely paradoxical tool. It allows for personal expression, yet rewards content that conforms to platform-specific tropes. On TikTok, health narratives are most successful when they adhere to a particular rhythm: before, during, after; problem, solution, gratitude. This narrative architecture invites empathy but often simplifies complexity.
In the context of breast reduction, this dynamic risks misrepresenting the full clinical landscape. The surgery, while effective, carries potential complications: loss of nipple sensitivity, poor wound healing, asymmetry, or dissatisfaction with appearance. The viral video, while emotionally impactful, largely omitted these considerations.
Medical professionals watching such videos often express concern that prospective patients may conflate anecdotal satisfaction with general safety. The American Society of Plastic Surgeons continues to emphasize the importance of preoperative counseling, informed consent, and individualized assessment—a message frequently lost in the compression of experience into seconds-long clips (source).
Gender, Pain, and the Performance of Justification
The stakes of breast reduction extend beyond physiology. They tap into a long history of societal discomfort with women’s pain, particularly when that pain is invisible or ambiguous. Large breasts are simultaneously sexualized and stigmatized; their medical consequences often trivialized.
That the video went viral is, in part, a testament to the legitimacy many women feel they must publicly perform to justify private decisions. The patient in question did not simply document her surgery—she narrated her suffering, framed her struggle, and validated her choice in ways designed to anticipate skepticism.
Such performance, while understandable, raises ethical questions: Should patients feel obligated to expose their vulnerabilities to earn empathy? Should medical legitimacy require social proof?
A Clinical Reckoning
In the days following the video’s ascent, several prominent physicians and health advocates used the momentum to call attention to insurance coverage gaps, outdated gender biases, and the absence of robust postoperative support for breast reduction patients.
Advocacy organizations such as The National Women’s Health Network have long argued for revising the criteria insurers use to assess medical necessity, especially in procedures linked to pain management and quality of life. The viral nature of the breast reduction video gives new energy to that campaign, providing a narrative anchor for policy arguments that might otherwise remain academic or bureaucratic.
It also raises practical questions for clinicians: How should physicians counsel patients who arrive with expectations shaped by algorithmic content? What responsibilities do providers have to help patients distinguish digital narrative from clinical norm?
Toward Digital Literacy in Medical Storytelling
Rather than vilify social media or discourage disclosure, healthcare institutions must learn to contextualize it. Physicians can discuss viral content with patients, not as threats to credibility but as opportunities for critical engagement. Academic medical centers might consider producing balanced short-form videos that explore procedures from multiple angles—physical, emotional, financial, and ethical.
Medical boards, too, may consider updating continuing education requirements to include modules on digital health literacy—not just for patients, but for providers navigating a landscape in which perception increasingly shapes practice.
Final Thoughts: From Empowerment to Expectation
The breast reduction video that captivated 25 million people was more than a personal testimony. It was a signal—of dissatisfaction with institutional care, of hunger for community validation, and of the enduring difficulty of making female pain legible in clinical and public spaces.
Yet the celebration of this digital milestone must come with caution. If we are to embrace patient storytelling as a cornerstone of contemporary health discourse, we must also guard against the erosion of nuance and the rise of visual expectation as medical standard.
Empowerment is not merely visibility. It is choice, complexity, and the right to act without the obligation to explain. The digital age offers a new frontier for that possibility—if we handle it with care.