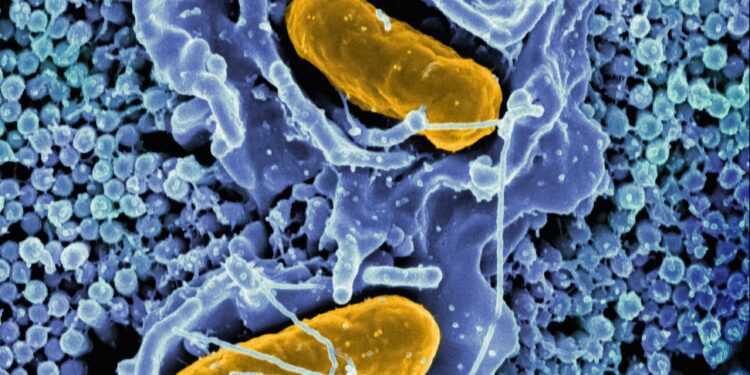
At the microscopic heart of every human cell lies a biological paradox: mitochondria, the tiny energy generators that power life, carry their own DNA—separate from the cell’s nucleus, and inherited only from mothers. These “powerhouses of the cell” have long fascinated biologists for their origin story, believed to be ancient bacteria that formed a symbiotic relationship with early eukaryotic cells. Now, they may be the center of one of the most radical medical interventions of the 21st century: mitochondria transplants.
The idea sounds futuristic—almost absurd. Remove faulty mitochondria from diseased cells and replace them with healthy ones, potentially restoring energy production in ailing tissues and reversing degenerative disease. Yet across university labs, startup biotech firms, and operating rooms, this once-fringe notion is becoming reality. Clinical trials are underway. Government funding is trickling in. Private investors are circling.
But so too are the skeptics.
This article investigates the scientific promise, commercial momentum, and ethical dilemmas of mitochondrial transplantation. Like many breakthroughs in regenerative medicine, this one arrives at the intersection of hope, hype, and hard questions.
From Theory to Therapy: The Science Behind the Transplant
Mitochondrial dysfunction is implicated in a wide range of conditions, from rare genetic disorders like Leigh syndrome and MELAS (mitochondrial encephalomyopathy) to more common diseases such as Parkinson’s, Alzheimer’s, and heart failure. Unlike nuclear DNA, mitochondrial DNA (mtDNA) is more vulnerable to damage, especially from oxidative stress. When mitochondria falter, cells lose their ability to generate ATP—the currency of energy—and organs begin to fail.
In concept, mitochondrial transplantation is simple: extract healthy mitochondria from donor cells and inject them into damaged tissue. These new mitochondria are then taken up by recipient cells, potentially rebooting their energy production machinery.
The first documented human mitochondrial transplant occurred in 2016, at Boston Children’s Hospital. Researchers led by Dr. James McCully injected healthy mitochondria into the hearts of infants suffering from ischemia-reperfusion injury. The results, though preliminary, were promising—showing increased heart function and reduced cell death.
Since then, preclinical studies have extended the approach to liver disease, stroke, and spinal cord injury. Animal models have demonstrated partial reversal of organ damage. In 2023, a small Phase I trial in Japan reported improved motor function in Parkinson’s patients who received mitochondrial infusions directly into affected brain regions.
“We’re essentially giving cells new batteries,” says Dr. Elena Ramirez, a cell biologist at the University of California, San Diego. “The body seems remarkably capable of integrating and utilizing these foreign mitochondria—though we still don’t fully understand why.”
Hope Meets Hype: The Commercial Push
Biotech companies have seized on mitochondrial transplantation as a potentially billion-dollar frontier. At least five startups—including Mitrix Bio, Cellvie, and ToleRx—have emerged in the past five years, each promising scalable platforms for mitochondrial isolation, preservation, and delivery.
Mitrix Bio, based in San Diego, is currently developing mitochondria-based therapeutics for neurodegenerative disease. The company has raised over $40 million in venture funding and recently received a Department of Defense grant to explore applications in traumatic brain injury.
“Our vision is to create a mitochondria bank—similar to how we have blood banks,” says CEO Dr. Thomas Benson. “Eventually, we see mitochondria as a therapeutic platform across many indications.”
But the road to that future is uncertain. Critics warn that the commercial ecosystem may be moving faster than the underlying science.
“We’ve seen this before—with stem cells, with gene editing,” says Dr. Maya Stone, a bioethicist at Johns Hopkins University. “There’s a rush to monetize before there’s consensus on safety or efficacy. That should worry everyone.”
Indeed, the regulatory landscape is fragmented. In the U.S., mitochondrial transplants currently fall into a gray area between cell therapy and organ transplantation. The FDA has yet to issue specific guidance, and clinical oversight varies widely.
Ethics and the Maternal Line
One of the thorniest issues surrounding mitochondrial interventions is the question of identity. Because mitochondria contain their own DNA, introducing donor mitochondria into a person’s body technically introduces foreign genetic material—however small. This raises difficult ethical and legal questions.
Nowhere is this more evident than in the context of mitochondrial replacement therapy (MRT), a procedure used to prevent the transmission of mitochondrial diseases from mother to child. In 2016, the U.K. became the first country to legalize MRT, under strict regulation. The first baby born via MRT—a so-called “three-parent baby”—was delivered in Mexico the same year, sidestepping U.S. law.
The technique involves replacing defective mitochondria in a mother’s egg with healthy ones from a donor egg, resulting in a child with nuclear DNA from its parents and mtDNA from a third person.
“This is not just a medical intervention,” argues Dr. Leena Prasad, a philosopher of science at the University of Cambridge. “It forces us to rethink our definitions of heredity, identity, and kinship.”
Opponents have called for stricter oversight or even moratoriums on MRT and mitochondrial transplantation in general, warning of potential long-term consequences—particularly if germline mtDNA is altered.
Supporters counter that for families affected by mitochondrial disease, the moral calculus is simple: a chance at a healthy child, or a life marked by suffering.
Follow the Energy: The Investment Landscape
Despite the uncertainty, investors remain bullish. The mitochondrial medicine market is projected to exceed $6 billion by 2030, driven by aging populations and the growing prevalence of metabolic and neurodegenerative disorders.
Pharmaceutical giants are beginning to take notice. In 2024, Roche partnered with a U.S. biotech firm to explore mitochondria-targeting therapeutics. Meanwhile, venture capital firms with a history in stem cells and CRISPR have quietly added mitochondrial startups to their portfolios.
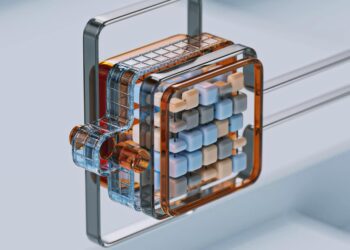
But unlike pills or biologics, mitochondria cannot be mass-produced in chemical factories. They must be harvested from cells—either autologous (from the patient) or allogeneic (from a donor). Scaling this process while maintaining mitochondrial integrity is no small feat.
“There’s a logistics challenge here,” says Dr. Ken Zhou, CTO at a startup developing cryopreservation methods for mitochondria. “You’re dealing with organelles that degrade quickly and must be delivered to the right tissues, at the right time, in the right dose.”
Until those hurdles are overcome, large-scale adoption may remain out of reach.
Conclusion: Mitochondrial Futures
In a world hungry for radical biomedical solutions, mitochondria transplants are an alluring proposition: a cellular reboot, a second chance, a new engine for old bodies.
But the path forward demands caution. As with many medical frontiers, what begins as hope can easily drift into hubris. The history of regenerative medicine is littered with cautionary tales—of therapies rushed to market, of hype outpacing data, of ethical corners cut in pursuit of glory or gain.
Mitochondrial transplantation may indeed change the landscape of medicine. But before we build a future powered by cellular batteries, we must ask hard questions about risk, regulation, equity, and intent.
After all, the most powerful forces in biology are not always the ones we understand best.