A single infusion of CAR-T cells can redefine a cancer patient’s prognosis while simultaneously igniting scrutiny over a $475,000 price tag. The June 2025 approval of Bristol-Myers Squibb’s cilta-cabtagene autoleucel for multiple myeloma has sharpened debates over how health systems can afford these curative promises without forsaking equity or sustainability (Reuters). At the same time, tumor-agnostic agents—drugs targeting rare genomic alterations regardless of tissue origin—such as Roche’s RO709, press payers and policymakers to reconcile value with cost.
The Promise and the Price
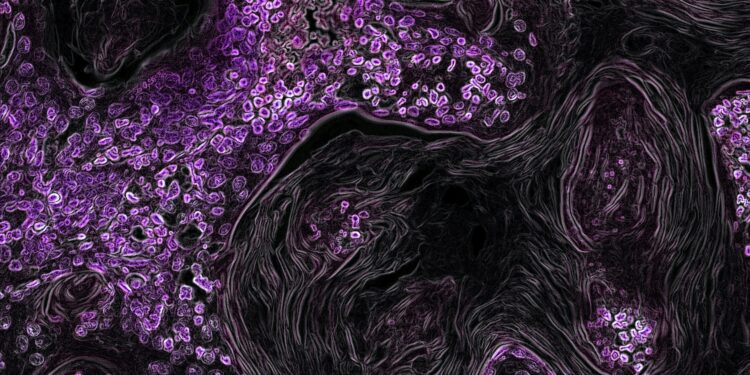
CAR-T therapies leverage patients’ own T cells, reengineered to seek and destroy malignant cells. Since the pioneering Kymriah approval in 2017, high-impact trials have reported durable remissions in refractory hematologic malignancies. Yet their unit costs—ranging from $373,000 for Yescarta to $475,000 for Kymriah—reflect manufacturing complexities and one-time administration models, prompting questions: Are these prices aligned with long-term value?
Health-technology assessments suggest they may be, at least in terms of quality-adjusted life years (QALYs) gained. A 2024 Pharmaphorum analysis noted that “prices based on current evidence are aligned with value to the patient,” yet cautioned that lifespan benefits beyond 15 years remain uncertain, complicating lifetime-horizon cost-effectiveness modeling (Pharmaphorum). Tumor-agnostic agents, such as those targeting NTRK fusions, carry list prices near $300,000 per year and rely on small, biomarker-driven trial cohorts, raising further questions about comparative effectiveness in real-world settings
Value-Based Pricing and Subscription Models
To reconcile high upfront costs with payer budgets, innovators propose value-based and subscription payment approaches. The PASTEUR Act, currently under congressional consideration, would establish subscription payments—“Netflix”-style contracts guaranteeing manufacturers fixed annual fees for unlimited patient access, decoupling revenue from volume and discouraging overutilization. Proponents underscore that such models “incentivize development of narrow-spectrum, high-value therapies” while capping payer liability.
Critics caution that subscription models require precise calibration of “fair” fees and robust outcome metrics. A white paper by Insights Bio notes that “indication-based pricing” may better reflect varying benefit magnitudes across cancer types, yet implementing this complexity challenges pharmacy and therapeutics committees (Insights Bio). Moreover, value-based agreements often hinge on adherence and follow-up data—difficult to collect for one-time, autologous treatments.
Payer Burden and Health-Policy Tensions
Payers confront mounting financial pressures. A Reuters briefing reports that U.S. policymakers are exploring price-linking mechanisms to international benchmarks for all medicines—CAR-T included—to restrain runaway costs (Reuters). Meanwhile, states that expanded Medicaid under the Affordable Care Act face daunting choices: covering these therapies could consume a disproportionate share of limited budgets, potentially crowding out other essential services.
Health-policy experts argue for dedicated funding streams or reinsurance pools for high-cost gene and cell therapies. The Innovative Health Policy Consortium proposes a national “high-cost therapies fund,” financed by modest surcharges on all prescription drugs, to equitably distribute fiscal risk. Such a fund would embody the ethical principle of justice—ensuring that no patient is denied transformative treatment solely due to payer constraints.
Patient-Assistance Models: Alleviating Out-of-Pocket Strain
Even with insurer coverage, patients often face substantial copays or coinsurance. Patient assistance programs (PAPs) run by manufacturers can mitigate these burdens but vary widely in eligibility criteria and benefit levels. A study in JAMA Oncology found that 18 percent of CAR-T recipients still incurred over $5,000 in out-of-pocket costs despite PAP support, leading some to forgo follow-up care and lab monitoring.
Ethical stewardship demands transparent, standardized assistance frameworks. The American Society of Clinical Oncology recommends that PAP eligibility hinge on objective financial assessments and that information be integrated into clinical pathways from the outset. Hospitals like MD Anderson have instituted financial navigation teams that proactively enroll patients in assistance programs and advise on insurance appeals, reflecting beneficence in patient advocacy.
Lived Experiences: Patients at the Heart of the Debate
Mrs. Thompson, diagnosed with refractory diffuse large B-cell lymphoma, received CAR-T therapy through a clinical trial. She recalls the relief of remission but also the anxiety of awaiting coverage decisions. “My insurer approved the treatment, but I had to fight for my travel and lodging costs”—expenses the PAP did not cover. Her case highlights the gap between therapeutic promise and real-world feasibility.
Similarly, Mr. Alvarez, treated with a tumor-agnostic TRK inhibitor for an NTRK-fusion sarcoma, recounts frustration when his insurer required additional rounds of imaging to justify continued coverage. “I felt I had to prove my worthiness,” he says, underscoring how administrative hurdles can erode patient autonomy and confidence.
Charting a Path Forward: Integrative Strategies
Addressing the cost-effectiveness challenge in precision oncology requires a multi-stakeholder approach:
- National Pricing Frameworks
Implement reference pricing for CAR-T and tumor-agnostic agents tied to demonstrated long-term outcomes, adopting a hybrid of value-based and international benchmarking. - Innovative Payment Models
Enact the PASTEUR Act or equivalent legislation to establish subscription or annuity payments, mitigating short-term payer shocks while rewarding sustained therapeutic success. - Dedicated Funding Mechanisms
Create federal or multi-state risk-sharing pools to underwrite extraordinarily high‐cost therapies, preserving general Medicaid and commercial plan solvency. - Standardized Patient Support
Mandate minimum PAP standards—uniform eligibility, coverage of ancillary costs, and transparent terms—to ensure equitable access without catastrophic financial exposure. - Robust Health-Technology Assessment
Encourage ICER and HTA bodies to issue annual updates on real-world performance and cost-effectiveness, informing iterative policy adjustments and coverage decisions.
Conclusion
Next-generation CAR-T therapies and tumor-agnostic agents stand at the vanguard of cancer treatment, offering curative potential once deemed impossible. Yet their remarkable power collides with sobering price tags and complex payer landscapes. Ensuring that these innovations fulfill their promise demands ethically grounded policies that balance beneficence, justice, and respect for patient autonomy. By pioneering value-based pricing, fortifying patient support, and forging sustainable funding streams, stakeholders can navigate the intricate junction of medical ethics, health policy, and individual patient experience—so that cutting-edge precision oncology reaches all who stand to benefit.