A clot moves in silence—until it kills.
That brutal, biological truth has haunted emergency rooms for decades. Strokes, heart attacks, pulmonary embolisms—these events often strike without warning, leaving little time for intervention. The human body gives few outward signs of the tiny, deadly formations that can trigger these catastrophes. But a breakthrough from the University of Tokyo may change that equation entirely, offering a glimpse into a future where real-time clot detection is not just possible, but practical.
A team of researchers, led by biomedical engineers and data scientists, has unveiled a non-invasive artificial intelligence (AI) system capable of monitoring platelet activity in real time. The implications are staggering: early warnings for deep vein thrombosis (DVT), better postoperative care, dynamic risk profiling for stroke patients, and a seismic shift in how cardiovascular events are diagnosed and prevented.
The Science Behind the Signal
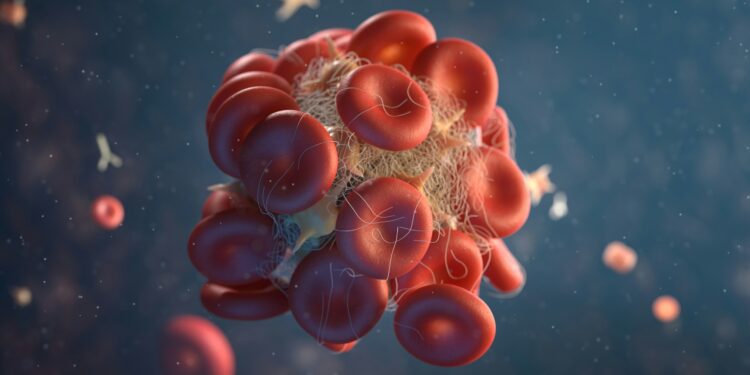
Platelets—the microscopic blood components responsible for clotting—are notoriously difficult to monitor. Traditional clot detection often requires imaging tools like CT scans, MRIs, or ultrasound, which are expensive, time-consuming, and reactive rather than proactive.
The Tokyo team’s AI-powered approach bypasses those limitations. Using a combination of high-speed microscopy and deep learning, their system tracks platelet motion and interaction in blood samples without needing invasive procedures. The AI component recognizes complex patterns in platelet aggregation—patterns that precede clot formation—before any physical symptoms manifest.
As detailed in Fox News Health, this system doesn’t just spot clots. It anticipates them.
Why This Breakthrough Matters
Blood clots are one of the leading causes of death globally. According to the Centers for Disease Control and Prevention (CDC), venous thromboembolism (VTE)—which includes deep vein thrombosis and pulmonary embolism—affects up to 900,000 Americans annually, resulting in 100,000 deaths. Nearly 25% of those who experience a pulmonary embolism die suddenly, often before any medical help can be administered.
The stakes are even higher post-surgery, during pregnancy, or in patients with chronic cardiovascular conditions. In these populations, timely detection is the difference between proactive treatment and fatal oversight.
Current diagnostics are either reactive (responding to symptoms after clots form) or probabilistic (assessing risk factors but lacking precision). This AI tool promises a third path: proactive, precise, and personalized.
How AI Transcends Traditional Diagnostics
Artificial intelligence excels at pattern recognition, particularly in high-dimensional data like cellular imaging. What a physician might miss, or what might require hours of lab analysis, an AI model can detect in milliseconds.
The Tokyo system leverages convolutional neural networks (CNNs), a subset of machine learning particularly adept at image analysis. By training on thousands of platelet behavior videos, the AI model “learned” to identify precursors to clotting events with remarkable accuracy. It can differentiate normal platelet activity from high-risk aggregations that suggest thrombogenesis is underway.
Critically, the system works in real time. This isn’t just data for the lab—it’s feedback that could guide immediate clinical decisions.
A Paradigm Shift in Preventive Medicine
Imagine a wearable device that monitors your blood and alerts you—or your physician—when you’re entering a pro-thrombotic state. Or a hospital dashboard where every post-op patient’s clotting risk is visualized dynamically. The shift from diagnostic response to predictive insight represents a new frontier in preventive medicine.
And the benefits are both clinical and economic. Early detection reduces emergency interventions, lowers hospitalization rates, and can save billions in downstream costs. For high-risk populations—such as those with atrial fibrillation, cancer, or immobility—the impact could be lifesaving.
Ethical and Clinical Questions on the Horizon
But the integration of such a tool into everyday healthcare is not without complications. Who is responsible for interpreting AI predictions? What happens when the AI flags risk, but the physician disagrees? Can real-time platelet tracking data be used in legal or insurance disputes?
Moreover, there are questions about accessibility. Will this tool be equitably distributed, or only available in high-tech urban centers? Will it further widen the diagnostic gap between rich and underserved populations?
As with all AI health breakthroughs, the ethical infrastructure must keep pace with the technology.
Regulatory and Commercial Considerations
The AI system is currently in preclinical trials, but commercialization is expected within five years. For FDA approval, it would likely fall under the SaMD (Software as a Medical Device) category. Given its real-time application and diagnostic potential, it may be subject to heightened scrutiny—particularly around accuracy, transparency, and interoperability.
Pharmaceutical and medtech companies are already eyeing the system for integration into anticoagulant management platforms. Hospitals and insurers see it as a potential tool for reducing preventable deaths and claims.
Conclusion: From Reaction to Anticipation
The blood clot has always been one of medicine’s most silent threats. With this new AI-powered system, we may finally have a way to listen for it.
This technology doesn’t just promise better diagnostics. It reimagines what medicine could look like when it’s built to anticipate rather than react. In doing so, it challenges long-held paradigms of clinical care, diagnosis, and risk management.
And perhaps most importantly, it offers a glimpse into a future where fewer people will hear the phrase, “If only we had caught it sooner.”
Because now, we just might.